This article first appeared in the Christian Research Journal, volume 20, number 1 (September-October 1997). For more information about the Christian Research Journal, click here.
SUMMARY
Over the past decade, governmental agencies, medical schools, influential voices in the media, and the public at large have seen a remarkable surge of interest in alternative medicine in the United States. While many therapies focus on unproven but otherwise spiritually neutral approaches (for example, nutritional supplements), others arise from or validate worldviews — especially the monism (“All is One”) of the New Age movement — that are hostile to the teachings of Scripture. The cultural developments that have brought alternative (still often called “holistic”) therapies into the cultural mainstream are complex and often understandable. However, a number of general cautions are still in order regarding this movement.
Twenty years ago a nurse tending to pediatric patients at Santa Monica Hospital handed me a rather unassuming publication bearing the title, Journal of Holistic Health. Along with more than 2,000 health-care professionals and other interested parties, she had just attended a conference in San Diego entitled, “The Physician of the Future.” In more ways than one, she had “got religion” at this meeting, and spoke with great enthusiasm about the new paradigm that would soon revolutionize our understanding of health and disease.
The future of health care, she explained, lay in the concept of “holism,” understanding the whole person — body, mind, and spirit — who was in fact a great deal more than the sum of several organ systems. It would become much more important to understand the patient who had the illness, not merely the illness that had the patient. Prevention, lifestyle, stress reduction, and self-awareness would displace the invasive and often destructive approaches — specifically, drugs and surgery — that had for so long dominated Western medicine. Eventually, we would begin to define health in more uplifting terms: not merely as the absence of disease, but as a state of increasing energy, productivity, insight, and personal transformation.
RISE OF HOLISTIC HEALTH
It sounded intriguing. After all, I was training as a resident in family practice — the specialty whose interest extended not only to the whole patient, but also to her or his family, work, relationships, and even the community where she or he lived. I glanced through the articles in this home-grown journal (which actually was a transcription of the previous year’s conference), and then began to read more carefully, with increasing concern. This movement appeared to have more on its mind than changing dietary habits, encouraging exercise, and coping with stress.
The conference director, David J. Harris, who bore the title Founder and President of the Association for Holistic Health, had rhapsodized in his opening remarks that this gathering “is part of a process that is bringing about a new way of thinking, a new science merged with religion.” James Fadiman, Ph.D., at that time Director of the Institute of Noetic Sciences at Stanford University, declared that “we are not primarily physical forms. We are primarily energy around which matter adheres.” Richard Svihus, M.D., President of the California Academy of Preventive Medicine, proclaimed that the holistic health movement “is desired by higher forces and consciousness within the universe.” Harold Bloomfield, M.D., a psychiatrist who had written the best-selling TM: Discovering Inner Energy and Overcoming Stress, extolled the benefits of Transcendental Meditation. Dr. Elisabeth Kübler-Ross, widely recognized as the world’s authority on the dying process, stated unequivocally that “death does not exist,” and that after transitioning from this life, you will have the opportunity “not to be judged by a judgmental God, but to judge yourself.” Many others with strings of initials after their names and impressive titles used engaging anecdotes that described healing through aligning the body’s invisible energies, developing psychic abilities, and — most important — altering, expanding, and transforming consciousness.
The pediatric nurse really had gotten religion — but not a gospel that would set well with Luke, the doctor who followed Jesus. It was, instead, a gospel better suited to Luke Skywalker, master of the Force, the impersonal energy allegedly pervading the universe. The holistic health movement, it turned out, appeared to be yet another banner under the “We are all energy / All is One / I am God / You are God / We are all God / Ain’t that great?” spirituality of the New Age movement. Such spirituality was storming the gates of Western culture and hoping to be welcomed with open arms.
In my subsequent explorations of the holistic phenomenon I attended two of the annual Association for Holistic Health conferences in San Diego. For the most part, the speakers were interesting, energetic, and sincere in their desire to promote health and healing, while the audiences were far more attentive than many I had observed at other medical conferences. These “total immersion” experiences left no doubt in my mind that the spiritual agenda of the “new medicine” — at least as presented by its most active proponents — was of utmost importance. Furthermore, a few direct questions to some of the speakers made it abundantly clear that this spirituality, which presented itself as generously inclusive of all religious traditions, did not in fact harbor warm and fuzzy feelings about such concepts as the sinfulness of humankind, Christ’s atoning death on the cross, or our need for individual repentance.
Ask a speaker about Jesus, and you would hear He was a Master Teacher, Enlightened Healer, Bearer of the Christ Consciousness, and so forth. Mention atonement, and you would be gently corrected, for Jesus demonstrated “at-one-ment” — an understanding of His (and our) unity with God. Bring up repentance, and you would be told that what we really need is enlightenment — a direct experience of our own divinity. Bear down on that distasteful event at Golgotha, and the air would suddenly become rather chilly.
Over the next several years, I both wrote and spoke of my concerns about the holistic health movement in a variety of settings, and while doing so, made a few observations:
First, a number of conventional medical practitioners were miffed over the idea that unorthodox healing systems were promoted as “treating the whole person” more effectively. Indeed, even the most narrowly focused subspecialist could truly keep the patient’s entire life in focus, attending to the mind and spirit as well as the body. Furthermore, there was no guarantee that an unorthodox practitioner might not see a patient as little more than a tangled wad of energy fields needing to be “balanced” through some esoteric formulation. (“Take these supplements/herbs that I have chosen for you through the most inscrutable and subjective criteria, and call me in the morning.”)
Second, many people — including committed Christians who would “go to the mat” over the interpretation of a grammatical detail in a passage of Scripture — appeared quite willing to lay critical thinking aside while dealing with unorthodox healing methods. “Does it work?” or, more specifically, “Does it make me feel better?” were often far more important questions than “Does it make any sense?” or “Is there any empirical proof?” or “On what world view is this healing system based?”
Third, the holistic health movement appeared to be having little impact on the practices of mainstream physicians. It had somewhat greater success among nurses, particularly with a specific healing technique known as therapeutic touch (see below).
Fourth, the “new medicine” also seemed to be making little headway within medical schools, government bodies, and insurance companies. Holistic health proponents repeatedly expressed a desire to leave the fringes and enter the cultural mainstream via research, public policy, and finance, but for many years this goal proved elusive.
Indeed, the persistent inability of holistic practices to gain widespread acceptance by the powers that be was undoubtedly a sore point for this movement for a number of years. Despite the grandiose optimism expressed during the San Diego conferences and others during the late 1970s and early 1980s, holistic health seemed to sputter through the 1980s, keeping itself alive primarily through paying clients who beat a path to the doors of unconventional practitioners. I concluded that there would always be holistic voices crying in the wilderness, but that our culture would probably keep them there.
My unspoken prediction, however, was proven wrong by some startling developments over the past few years. A dramatic turnabout has brought the gamut of holistic therapies — including those with New Age and Eastern mystical flags fully unfurled — squarely into the mainstream of American culture under a new banner: alternative medicine. Some proponents prefer the more conciliatory term complementary medicine, while a few describe themselves as promoters of integrative medicine, seeking to unite all forms of health care into a coherent system. Alternative medicine, however, is the most widely used term.
ALTERNATIVE MEDICINE TODAY
It is difficult to pinpoint when or how this reversal began. Promoters of alternative health care would likely argue that this movement hasn’t actually enjoyed a revival, but that it has been alive and well all along, and that the power elites of the press, government, and medicine have only recently noticed. This idea is supported to some degree by a now-famous 1993 article in the New England Journal of Medicine, a publication not exactly known for tabloid excesses.
The report detailed the findings of a 1990 survey of health care utilization in the United States, suggesting that more than 30 percent of American adults availed themselves of at least one form of alternative therapy that year, paying an estimated 425 million visits to providers of such treatments — about 40 million more than the number made to primary care physicians! The tab for this care was nearly $14 billion, of which more than $10 billion was not covered by insurance and thus was paid out of pocket. The survey indicated that unconventional therapies were used mostly for chronic rather than life-threatening conditions, that most people using these alternatives didn’t discuss them with their physicians (no great surprise since conventional practitioners tended to dismiss such options with eye-rolling disdain), and that the elderly represented a significant proportion of the clientele.1
A RECENT SURGE IN PUBLIC INTEREST
It would not be surprising if a survey taken today showed even more widespread involvement in alternative practices. Recent indications of a surge in public interest include the following:
A Time cover story entitled “Faith and Healing” (24 June 1996) painted its subject with broad strokes, encompassing traditional faith in God, meditative techniques, and biochemistry. It described “controlled studies” designed to determine whether patients who were the recipients of prayer — defined in a variety of ways — fared better than others.
A bumper crop of books on alternative therapies now line the shelves of the “Health and Medicine” section of the typical neighborhood bookstore. No longer limited to the off-label and self-published material that was once the staple of New Age outlets, the newer titles come from mainstream publishers, and place unconventional treatments on equal footing with Western medicine. One prominent example is The Medical Advisor: The Complete Book of Alternative and Conventional Treatment,2 published last year by Time-Life Books. This handsome volume describes health problems in encyclopedic detail, noting for each the conventional medical approach and then listing several alternatives: ancient Chinese, homeopathic, herbal, and so on.
The Public Broadcasting System (PBS) has repeatedly broadcast presentations of alternative healing. Bill Moyers’s 1993 series, Healing and the Mind, attracted almost twice the normal PBS viewing audience. Andrew Weil, M.D., a popular author who now teaches “Integrative Medicine” at the University of Arizona School of Medicine, has offered articulate distillations from his book Spontaneous Healing on a program of the same name. Deepak Chopra, M.D., a publishing hot-ticket and America’s foremost purveyor of India’s ancient healing system known as ayurveda, captivated viewers in the PBS specials, “Body, Mind and Soul: The Mystery and the Magic” and “The Way of the Wizard.”
Websites devoted to alternative therapies abound on the Internet. If one tells the Yahoo search engine to look for “alternative medicine,” he or she will be escorted to more than 200 sites, many of which provide links to dozens of others. On the other hand, cautionary notices and critical analyses by organizations such as the National Council against Health Fraud and the Committee for the Scientific Investigation of Claims of the Paranormal (CSICOP, a humanist think tank that publishes Skeptical Inquirer) are few and far between.
Periodicals promoting alternative therapies are now available both for the general public (for example, Natural Health) and health care providers. The monthly journals Alternative and Complementary Therapies and Alternative Therapies in Health and Medicine contain articles and studies of variable quality, which in some cases (unlike standard medical journals) freely wade into metaphysical and promotional material.
The most striking foray into the realm of conventional medicine occurred last November when American Family Physician, the official journal of the American Academy of Family Physicians (normally a reliable resource), published as its cover article, “Alternative Medicine and the Family Physician.”3 Authored by James M. Gordon, M.D., who directs the Mind-Body Center in Washington, D.C., the article offered a bland overview of alternative care, admonished family physicians to “convey a sensitive acceptance and an openness to….their patients’ interest in alternative therapies,” and encouraged practitioners to explore this realm themselves — starting with Gordon’s own book, Manifesto for a New Medicine. An accompanying editorial strongly endorsed physician involvement in alternative therapies, and a duplicable information sheet did likewise for patients. Nowhere in these materials was there a note of caution or concern about any of the approaches mentioned.
NEW LINKS WITH CONVENTIONAL MEDICINE
Manifestations of increasing interest in alternative health care have not been limited to the general public and news media. In 1991, Congress mandated the formation of the Office of Alternative Medicine (OAM), now permanently established within the National Institute of Health (NIH). OAM’s mission is to “encourage and support the investigation of alternative medical (AM) practices, with the ultimate goal of integrating validated alternative medical practices into health and medical care” (emphasis added).4 To this end, 10 exploratory centers have been established at institutions such as the University of Minnesota Medical School, Stanford University, and Columbia University’s College of Physicians and Surgeons. NIH guidelines for these centers call for “a systematic analysis of alternative treatments and their effect on major diseases, health, and wellness.”5
It remains to be seen whether the centers, each of which will focus on a specific health care issue, will approach alternative therapies with open arms along with open minds. Columbia-Presbyterian Medical Center, for example, has already established the Richard and Hinda Rosenthal Center for Complementary and Alternative Medicine, the first of its kind at an American medical school. A quote in the Rosenthal Center’s brochure from Woodson Merrell, M.D., sounds less than dispassionate: “The fact that medical schools are beginning to incorporate alternative modes of healing into their curriculum is a major step in medical education. It is very exciting.”
The enthusiasm for alternative medicine displayed by those involved with OAM certainly raises some doubt that its programs will provide evenhanded analysis of the therapies they study. Representative John E. Porter (R-Ill), Chairman of the Labor, Health and Human Services Education Subcommittee, which oversees funding for NIH, not only supports OAM but also sees it as fulfilling a specific mission: “As I see it, the most important contribution the OAM can make to the practice of medicine is to provide that link between alternative and conventional medicine….Therefore, it is important to continue making contacts on Capitol Hill and to deliver the message: alternative medicine is integral to biomedical research, provides effective results, and is a priority for spending decisions.”6 James Gordon, M. D., who wrote the above-noted Manifesto for a New Medicine, also serves as Chairman of the Program Advisory Council for OAM.
WHY THE INTEREST?
What might explain this surge of interest in alternative therapies? There are many possible reasons, but the heart of the matter is this: for all of its technological prowess, especially with acute and critical conditions, Western medicine continues to bump against the limits of its effectiveness when dealing with many disabling chronic conditions — especially those related to aging, such as degenerative arthritis — as well as complex diseases, such as cancer and HIV/AIDS. A massive tide of “baby boomers” is now facing mid-life and menopause, and, having challenged the status quo at every stage of life, this generation is not about to accept a “just deal with it” approach to the health problems of its golden years.
Moreover, stress and common lifestyle-induced problems, such as chronic fatigue and depression, do not always find sympathetic ears and definitive solutions in the doctor’s office. Many conventional practitioners drive large numbers of people to alternative therapists by spending as little time as possible with their patients and by clinging to outmoded authoritarian roles (“I know what’s best for you, so don’t ask me those irritating questions.”). Alternative practitioners may listen more attentively to their patients, and they frequently promote themselves as encouraging a more collaborative relationship.
Yet encouraging mutual respect, open communication, and informed decision-making are not the exclusive province of alternative therapies. In fact, many conscientious doctors within the conventional model have inadvertently contributed to the popularity of alternative therapies by candidly admitting the limits of their capabilities and carefully explaining the pros and cons of treatment options. Maintaining this evenhanded approach requires using words such as “might,” “maybe,” and “I don’t know.” Furthermore, an increasing — and appropriate — emphasis on informed consent over the past few decades requires physicians to present both the risks and the benefits in connection with a given medication or surgery.
As a result, in many situations a physician may not be able to bring the power of positive expectation to bear on the patient’s problem. Alternative therapies, on the other hand, are typically brimming with optimism, often inversely proportional to their ties to reality. After hearing more than one doctor say, “I don’t know what is causing your problem or what we can do about it,” someone with a complex illness may feel a breath of hope when the alternative practitioner announces, “I can find out why you feel so poorly, and I have a specific plan that will get you on the road to recovery.”
Other reasons for the rising interest in alternative therapies include:
(1) The appeal of “natural” approaches — often touted as “helping the body to heal itself” — over drugs and surgery. There is no question that ounces of prevention are better than pounds of cure, and positive lifestyle choices (regular exercise, prudent eating habits, and avoidance of harmful substances) are very likely to reduce medical problems in the future. But all too often the term “natural” is misapplied to bizarre, illogical treatments or the use of huge (and unnatural) amounts of vitamin and mineral supplements. Eating a variety of wholesome foods every day is natural; taking a tackle-box full of supplements is not.
(2) The current cultural enthronement of “choice” — the need to have options, to “have it my way” — has become a national credo. The word “alternative” implies that there is a choice to be made regarding health care, as opposed to simply following “doctor’s orders.”
(3) Skyrocketing costs, especially related to high-tech procedures and expensive medications, continue to plague the conventional health care system. Because alternative therapies tend to be relatively lowtech and often stress activities that the individual can do for himself or herself, some managed care/HMO systems are investigating their potential for lowering health care bills.
(4) A deep and widespread spiritual hunger. A number of therapies serve as a gateway to spiritual technologies and world views that address needs for meaning, knowledge, and power.
So what is the problem with alternative medicine? Before addressing that question, it is important to state what is not at issue.
(1) Turf battles. As a conventional, Western-trained practitioner, I can readily affirm that any concerns that I or others raise about alternative practices are not driven by possessiveness for patients or the income derived from them. Furthermore, it is important to counter an allegation that circulates with variable fervor in alternative circles: The A.M.A., the “medical establishment,” the pharmaceutical industry, or some other nefarious conglomerate is suppressing effective alternative treatments — especially for cancer — as part of an evil scheme to “keep people sick” so that billions of dollars can be made treating them. This paranoid delusion has as much basis in reality as a Stephen King novel, and begs the obvious question: What do these plotters do when any one of them — or a loved one — develops cancer? This rumor needs to be given a decent burial.
(2) Optimizing lifestyle. Many alternative devotees pay close attention to their daily living habits and make wise decisions (although sometimes for odd reasons). Primary care physicians are always delighted to have “low maintenance” patients who make wholesome dietary choices, exercise regularly, shun harmful substances, and deal effectively with life’s stresses. If this were the sum of alternative or holistic health, there would be little to be concerned about and much to applaud.
(3) Effective treatments based on rational thinking and solid research. One of the potential benefits of the Office of Alternative Medicine is the sponsorship of studies to separate alternative wheat from chaff. For example, the Rosenthal Center is conducting a double-blind, randomized study to determine whether a specific Chinese herbal preparation is effective in treating menopausal hot flashes. If such research validates this particular herbal remedy as a useful therapeutic tool and provides guidelines for its appropriate use, many women will be grateful beneficiaries.
(4) Recognizing the spiritual dimension to health. Human beings are indeed more than a collection of complex biochemical reactions, and their spiritual values can play an important role in both health and illness. Research psychiatrist David Larson, M.D., at the National Institute for Healthcare Research has collected a large number of studies that indicate that regular churchgoers are, among other things, more likely to have a reduced risk of coronary artery disease, lower blood pressure, less depression, and fewer anxiety-related illnesses. Furthermore, these benefits appear to be independent of lifestyle decisions (such as abstaining from smoking) that might arise from spiritual commitments. However, a number of alternative therapies and conceptions of health embrace metaphysical orientations overtly hostile to the teachings of the Old and New Testaments.
PROBLEMS WITH ALTERNATIVE MEDICINE
Presenting a detailed critique of even a sampling of alternative therapies is beyond the scope of this article. The following basic problem areas are presented, however, as a caution to those involved in this realm.
Excessive promoting. To say that the realm of alternative medicine is characterized by optimism is an understatement, and undoubtedly much of its success is due to its unabashedly positive outlook. Unfortunately, this buoyancy tends to pervade even its “serious” journals, such as Alternative and Complementary Therapies, raising doubts about the willingness of alternative practitioners to engage in any serious form of peer review. For all of its faults, Western medicine has progressed by honoring skepticism and doubt, and by demanding that the efficacy of its interventions be validated by controlled studies. Even the extensive advertising to physicians and patients by the pharmaceutical industry is governed by strict guidelines regarding claims that can be made about a given product.
There is no similar oversight for the myriad of herbal formulations, supplements, homeopathic remedies, and other concoctions heavily promoted in magazines, health food stores, and infomercials. (On weekends, some Christian radio stations literally transform into alternative therapy flea markets, without any apparent regard for the credibility of the material emanating on their airwaves.) Expansive claims abound for restoring energy, improving digestion, and solving a variety of poorly defined ailments (“heart problems,” “kidney disease,” etc.), all unspecified. Testimonials and anecdotes serve as proof positive, and any attempt by the Food and Drug Administration to bring some order to this Dodge City are met with howls of protest from merchants and buyers alike.
“Everything you know is wrong.” A number of alternative therapies also postulate alternative realities — convoluted explanations of how things work in the human body (or the universe in general) that are totally at odds with the most basic facts of physiology. These are politely referred to in OAM literature as “traditional and ethnomedicine therapies,” and include such far-flung systems as ancient Chinese medicine and its offshoots (classical acupuncture and acupressure, among others), ayurvedic medicine from India, and homeopathy. Each operates as a self-contained system with its own internal logic, and while they seem to coexist happily under the “big tent” of alternative medicine, each is quite incompatible with the others. Questions about the validity of each system’s basic assumptions are usually deflected with references to the “accumulated wisdom of thousands of years of careful observation” or the “hundreds/ thousands/millions of treatment successes/satisfied customers” or (best yet) the “many scientific studies documenting the effectiveness of _____ .” What proof is there, for example, for the ancient Chinese notion that invisible energy called ch’i circulates in equally invisible channels called meridians, and that disease results from disturbances in that flow?
The reference to many scientific studies is the most ironic because the methodology of modern scientific inquiry clearly came up with an understanding of health and disease that bears absolutely no resemblance to the precepts of these systems. For a quick reality check, imagine for a moment the reception that would greet an “alternative system” of mechanical engineering, aeronautics, or navigation based on ancient Eastern mysticism. Imagine, for that matter, an effort by your local emergency room to revive Hippocrates’s doctrine of the “four humours” as the basis for diagnosis and treatment.
Postmodern thinking. The fact that fanciful healing systems thrive in industrialized nations is partly due to the fact that postmodernism has penetrated Western cultures to a significant degree. This world view rejects both scientific rationalism and biblical notions of absolute truth, and substitutes for them intense subjectivism: “Truth is defined by my experience/my feelings/my understanding.” The scientific method and all that it entails — rational hypotheses, logical deductions, controlled studies, and revising one’s opinions based on this arduous process — are seen as no more valid a way of understanding the world than any individual’s mystical experiences or intuitive hunches. Any claim that one approach to obtaining knowledge might, in fact, be better than another, or that there is any absolute truth — especially a transcendent God who is the truth — is viewed as a power play, an attempt by one person to suppress and oppress someone else.
One alternative well suited to a postmodern culture is therapeutic touch, a practice that has continuously gained in popularity among nurses since its introduction in 1975 by New York University Professor Dolores Krieger, R.N., Ph.D. Now taught at more than 80 universities and hospitals, therapeutic touch purports to detect and adjust invisible energies supposedly flowing within and emanating from the human body. This involves entering a meditative state, moving the hands slowly about two inches above the patient’s skin in an effort to detect subtle sensations such as tingling or heat, using the hands to “sweep away” excess energy that might have been detected, creating mental images of desirable energy states, and then directing these images to the patient through the hands.
Aside from its misleading title (it should be “therapeutic nontouch”), the utter lack of objective validation for an invisible human energy field and the spectacular subjectivism of its technique (how in the world can anyone tell whether someone is doing it “correctly”?), therapeutic touch possesses a mystical heritage that should chill any practitioner who possesses even the faintest belief in the veracity of Scripture. Dr. Krieger’s book The Therapeutic Touch makes it clear that she views Eastern mysticism and the Hindu concept of a universal energy called prana as the cornerstone for her therapy. She writes, “The idea that prana might be transferred from one individual to another may not be so readily apparent to us unless we have gotten into the practice and literature of hatha yoga, tantric yoga, or the martial arts of the orient.”7
Whenever therapeutic touch is called into question, a chorus of protest — even from some Christian nurses who embrace this technique (often erroneously equating it with the “laying on of hands” in the New Testament) — is a virtual certainty. But regardless of the benign intentions of its practitioners and its frequent proclamations of validation by some scientific studies, this technique represents a florid invasion of Eastern mysticism into the corridors of Western medicine.
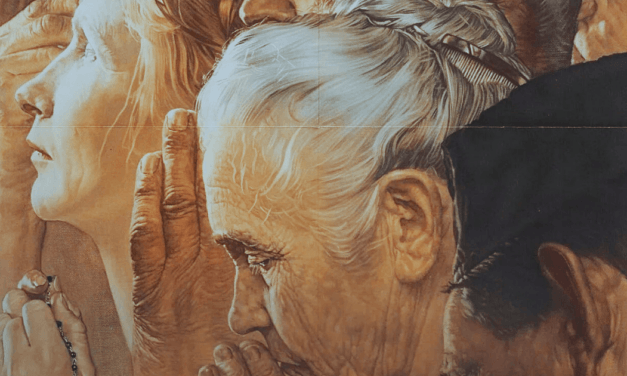
The hijacking of prayer. Alternative medicine has embraced prayer as a healing modality, and in doing so, it has repeatedly fooled even mature Christians. This has occurred in two ways. One is exemplified by a 1988 study reported in the above-noted Time article, “Faith and Healing.” Nearly 400 patients in the coronary care unit at San Francisco General Hospital were randomly assigned to two groups. Patients in the “experimental” group were prayed for by born-again Christians, while those in the “control” group were not. Neither group of patients knew this was being done. Lo and behold, the prayed-for group had one-third the number of complications. Some Christians who become aware of such studies are thrilled: Finally science is validating what the Bible says about prayer.
But is God Almighty, Maker of heaven and earth, an appropriate subject for a controlled study? Is the potter going to be subject to a randomized protocol of the clay? Is prayer merely a form of spiritual technology? This type of experiment encompasses the worst of both worlds — misdirected science and presumptuous theology — and indirectly validates the misguided assumption (prevalent even among many Christians) that prayer is a cosmic call button, in response to which an omnipotent butler automatically fulfills human desires.
The other fake-out, involving some inventive verbal sleight of hand, is exemplified by the writings of Larry Dossey, M.D., author of the bestselling Healing Words and the more recent Prayer Is Good Medicine. Dossey is widely quoted even in reputable Christian publications because of his encouraging thoughts about the role of prayer in healing. But his notions of prayer extend well beyond the basic concept of communication between a human being and the omniscient, omnipotent, and loving Creator. He views prayer as a “nonlocal” extension of human consciousness: “Prayer actually enlarges the reach of human consciousness. It is a way for us to transcend our physical limitations — to be nonlocal, like gods.”8 It doesn’t matter much whether one prays to Jehovah or to the entire universe, or merely extends positive thoughts in another person’s direction. To him it’s all prayer and it’s all good.
In the Bible, however, the importance of worshiping and honoring the one true God is of paramount concern. It does matter to whom we pray, and with what attitude. Furthermore, doing so requires that we have a clear understanding that God is God, and we aren’t — which brings us full circle to the last and most serious problem with alternative medicine.
Health is godhood. As noted at the beginning of this article, the holistic health movement of 20 years ago embraced a concept that was in fact deeply embedded in many of its therapies: “Matter and energy are different forms of the same reality. We are all congealed energy — the same energy that fills the universe, which some call God. Therefore we are God.” Alternative medicine in the 1990s has in no way distanced itself from this world view.
Perhaps the most successful proponent of this philosophy in the United States is Deepak Chopra, M. D., author of numerous best sellers including Ageless Body, Timeless Mind and The Way of the Wizard, ubiquitous endorser of other alternative medicine books, and favorite of PBS viewers and movie stars. Originally trained in Western-style endocrinology and once the prime promoter of Maharishi Mahesh Yogi’s foray into health care, Chopra is now in command of his own Chopra Center for Well Being in La Jolla, California.
Chopra shouts the virtues of ayurveda from the media housetops. He promotes the notion that we are all local nodes in the infinite, universal energy field (call it “God” if you wish): “All of us are connected to patterns of intelligence that govern the whole cosmos. Our bodies are part of a universal body, our minds an aspect of a universal mind.”9 So when the physical body dies, we have nothing to fear. As he explains in a recent column in Natural Health, “Once our physical body disintegrates, we go through a period of deep slumber as an astral body….after which we gradually awaken to experiences that we need to work out.” Eventually we “get in touch with our karmic software” and then re-emerge on the physical plane with a higher level of awareness. “With each cycle of life and death we move into a higher or more refined vibratory frequency of consciousness.”10
THE SAME OLD LIE
This is, of course, the old reincarnation shuffle, presented to reassure readers of this alternative health magazine that all will be well during their next several appearances on earth, until ultimate health — a final unity with the “universal mind” — takes place. Obviously, in such a scenario there is no need for God to have become a man to become a ransom for many, and no need for repentance, but only a need for each of us to experience our godhood.
These are yet another presentation, in all of their primal seduction, of the two most basic lies ever told to human beings: “You shall be as gods, and you will not die.” Unfortunately, despite an abundance of optimism and good intentions, many who are involved in alternative medicine — especially those who claim to detect and manipulate invisible energies — are unwittingly distorting God’s true identity as creator and Lord, and our true identity as creatures who need first to be saved by Him and then to serve Him.
Paul Reisser, M.D., is a family physician in private practice in Southern California. He is the coauthor of several books, including New Age Medicine (InterVarsity Press, 1988) and the upcoming Focus on the Family Complete Book of Baby and Child Care (Tyndale). He is a member of the Focus on the Family Physicians Resource Council and medical commentator for the radio broadcast “Family News in Focus.”
NOTES
- D. M. Eisenberg, R. C. Kessler, C. Foster, F. E. Norlock, D. R. Calkins, and T. L. Delbanco, “Unconventional Medicine in the United States: Prevalence, Costs and Patterns of Use,” New England Journal of Medicine 328 (1993): 246-52.
- The Medical Advisor: The Complete Book of Alternative and Conventional Treatment (Alexandria, VA: Time-Life Books, 1996).
- James M. Gordon, “Alternative Medicine and the Family Physician,” American Family Physician 54,7 (1996): 2205,12
- “Exploratory Centers for Alternative Medicine Research,” NIH Guide, vol. 23, no. 15 (RFA: OD-94-004), 15 April 1994.
- Ibid.
- John E. Porter, “OAM Funding: A Shared Responsibility,” Alternative Therapies in Health and Medicine 1,3 (1995): 80.
- Dolores Krieger, The Therapeutic Touch: How to Use Your Hands to Help or Heal (Englewood Cliffs, NJ: Prentice-Hall, 1979), 13.
- Larry Dossey, Prayer Is Good Medicine (New York: HarperCollins Publishers, 1996), 79.
- “Emperor of the Soul,” Time, 24 June 1996, 68.
- Deepak Chopra, “Soul Searching,” Natural Health, January/February 1997, 192.